As physicians, some of us love to read the latest journal publication while some of us don’t give a s@#!. Those in the latter category are more than happy to get the information at conferences or journal clubs in due time. There’s nothing wrong with these people…in fact, it could be argued this is a healthier approach than being addicted to your wireless device or computer waiting for the newest publication!
But for those of us who do get turned on by reading then talking about the newest publication the day it comes out “Epub ahead of print”, it can be a daunting task to stay up to date.
In our world where we’re exposed to up to the minute Twitter feeds, blog posts or push notifications, we can easily become overloaded and inundated with how to manage this information. The challenge is particularly difficult with journal publications. I admit, that I really enjoy reading the latest research data and while that doesn’t make me a bad person…it arguably makes me a less attentive husband (one woman’s opinion).
Are there any strategies for improving information intake and staying up to date with recent research? I don’t think this area is well taught in medical school or residency, partly due to the fact it’s a brand new method of information acquistion. Also, it’s rapidly changing with new sites and apps coming all the time.
I follow a few different journal topics including emergency medicine related, critical care, general medicine and medical education. Overall, this probably results in about 15-20 journals per month. I don’t read every article, nor do I read every abstract but I routinely read through table of contents or titles to make sure I’m staying up to date.
I’ve been thinking about this recently and while this post isn’t intended to be comprehensive, it does offer a few strategies that I’ve used to ensure I’m reading the newest evidence (any mention of a product/app below is only because I’ve found them helpful…I take no money from anyone). The following are in no particular order of preference. And if there’s an app or strategy I’m missing, please comment and I’ll add it to the post!
Here we go.
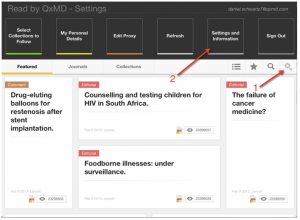
QxMD “Read”: I just started using this app and I really like it and I highly recommend it for any physician trying to keep up with the medical literature. And it’s FREE! Anyways, it’s a Canadian company that “provides a single place to discover new research, read outstanding topic reviews and search PubMed“. It allows you to sign up through your library Proxy account and access PDFs for any medical journal that your library has available. If your university isn’t supported, email them, I believe they are really working hard to add new institutions. The key component for this app is the user can select which journals they want to receive regular updates from and easily access. Here’s a great review of the product. For those using Android/non-Mac products I don’t think its available for any other platform than Apple (I only use Mac so I can’t confirm this).
Settings page for “Read”
Main interface used when reading articles
Feedly: I also highly recommend this! and it syncs with GoogleReader which inexplicably is getting shut down. This program provides regular updates to any journal you wish to add to your list. The benefit to this approach is that it syncs well across platforms (both mobile and desktop) and it also houses all of your non-medical blogs and news sites. The difference between Feedly and QxMD is the latter offers a much easier route to read the PDF. Feedly simply provides you with the abstract then its up to you to figure out your own access method.
Subscribe to a journal’s table of contents (TOC): Most journals allow you to provide your email so that every time a new volume is published, the TOC arrives in your inbox. This is how I started following journals though depending on the number of emails you receive (and the number of journals you follow), this process can easily overwhelm.
Example of “The Lancet” Table of Contents email
Subscribe to programs such as Journal Watch or InfoPOEMs (from Cdn Med Assoc): Essentially these organizations review the literature (typically 1-2 months behind) and send brief summaries of selected articles. This isn’t comprehensive and they’re not always free (e.g. Journal Watch) but it does help you find out about papers that maybe you wouldn’t have read. I use these methods then I download the article myself using my University library account. But it is a bit more labor intensive than Feedly or QxMD.
Follow an up to date medical blog. For those in emergency medicine/critical care, lifeinthefastlane.com is a must. The authors of this blog provide high quality, regular, up to date information about new publications that will interest EM physicians. Sign up to their LITFL review and they outline some of the newest journal articles out there. In addition, they link you up with all the most recent blog posts from around the EM world.
For those interested in medical education – I highly recommend a new blog “Medical Educator 2.0” that compiles medical education (and general education) related topics from sources around the world. Ali Jalali is a medical educator at the University of Ottawa (and happened to be a professor of mine in med school) and he puts together a very high quality site. If you subscribe then you’ll get regular emails when a new version/updates are posted.
Download each journal’s app: Great if you only read 1-2 journals but not sure how useful this is if you’re looking for regular updates from a broad range of journals. Here’s a list of journal apps for download.
Twitter: Either sign up and follow a journal’s twitter account (e.g. @EmergencyMedBMJ) or follow individuals that often retweet or post comments about new articles. This approach really maximizes the power of crowds and can make reviewing new articles much easier. On Twitter, you can also follow hasthtags like #meded and #FOAMed.
So those are a few strategies that I use. I welcome feedback and suggestions that I’ve missed. I’m happy to update this post with any ideas that you feel should be included.